CARTILAGE RESTORATION
Exploring Cartilage Restoration in Orthopedics
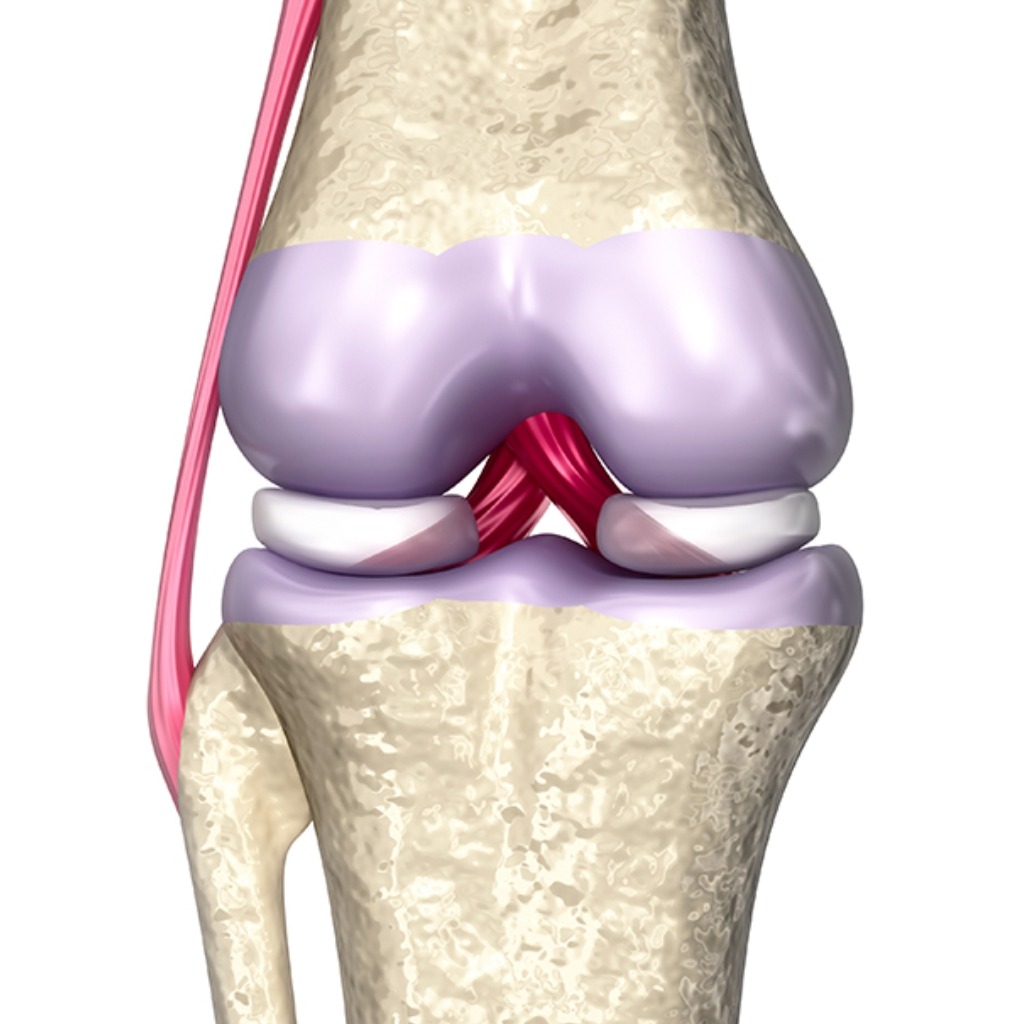
Cartilage restoration is an innovative orthopedic procedure aimed at repairing damaged or degenerated cartilage in joints, particularly the knee. Cartilage plays a crucial role in cushioning and facilitating smooth movement within joints, and injuries or conditions that compromise its integrity can lead to pain, stiffness, and reduced function. Cartilage restoration techniques offer hope for individuals seeking to preserve joint health and mobility. Let’s delve into the world of cartilage restoration and its impact on orthopedic care.
Understanding Cartilage Restoration
Cartilage restoration refers to a variety of surgical techniques and procedures designed to repair or regenerate damaged cartilage in joints. These procedures are typically indicated for individuals with focal cartilage defects or early-stage osteoarthritis, where the cartilage damage is localized and limited in extent.
Indications for Cartilage Restoration
Cartilage restoration procedures may be recommended for individuals with:
- Focal cartilage defects: Small, localized areas of cartilage damage typically caused by injury or trauma.
- Osteochondritis dissecans: A condition characterized by the separation of cartilage and underlying bone fragments within a joint.
- Early-stage osteoarthritis: Degenerative joint disease affecting specific areas of the cartilage surface.
Cartilage Restoration Techniques
Microfracture: Involves creating tiny holes in the subchondral bone to stimulate the formation of a blood clot, which serves as a scaffold for the growth of new cartilage-like tissue.
Autologous Chondrocyte Implantation (ACI): Involves harvesting healthy cartilage cells (chondrocytes) from a non-weight-bearing area of the joint, growing them in a laboratory, and then implanting them into the cartilage defect during a second surgical procedure.
Osteochondral Autograft Transfer (OAT) and Osteochondral Allograft Transplantation: Involve transferring healthy cartilage and underlying bone from a non-weight-bearing area of the joint (autograft) or a donor (allograft) to fill the cartilage defect.
Matrix-induced Autologous Chondrocyte Implantation (MACI): Similar to ACI, but the harvested chondrocytes are seeded onto a biocompatible scaffold or matrix, which is then implanted into the cartilage defect.
Rehabilitation and Recovery
Following cartilage restoration surgery, patients undergo a structured rehabilitation program tailored to the specific procedure and individual needs. Rehabilitation aims to protect the healing tissue, improve joint mobility, strengthen surrounding muscles, and gradually return to normal activities. Physical therapy plays a crucial role in optimizing outcomes and facilitating long-term joint health.
Benefits of Cartilage Restoration
- Pain Relief: Cartilage restoration procedures can help alleviate joint pain and discomfort associated with cartilage defects or early-stage osteoarthritis.
- Improved Function: By repairing or regenerating damaged cartilage, these procedures can improve joint function, stability, and range of motion.
- Delaying or Preventing Joint Degeneration: Cartilage restoration may help delay or prevent the progression of cartilage degeneration and the need for more invasive interventions, such as joint replacement surgery.
Conclusion
In summary, cartilage restoration represents a promising avenue for preserving joint health and function in individuals with focal cartilage defects or early-stage osteoarthritis. Through a combination of surgical techniques, rehabilitation protocols, and ongoing monitoring, orthopedic specialists strive to optimize outcomes and improve quality of life for patients undergoing cartilage restoration procedures. By harnessing the body’s innate capacity for tissue repair and regeneration, cartilage restoration offers hope for individuals seeking to maintain an active and pain-free lifestyle despite cartilage damage in their joints.